Immune thrombocytopenia (ITP)
Our ongoing research focuses on ITP
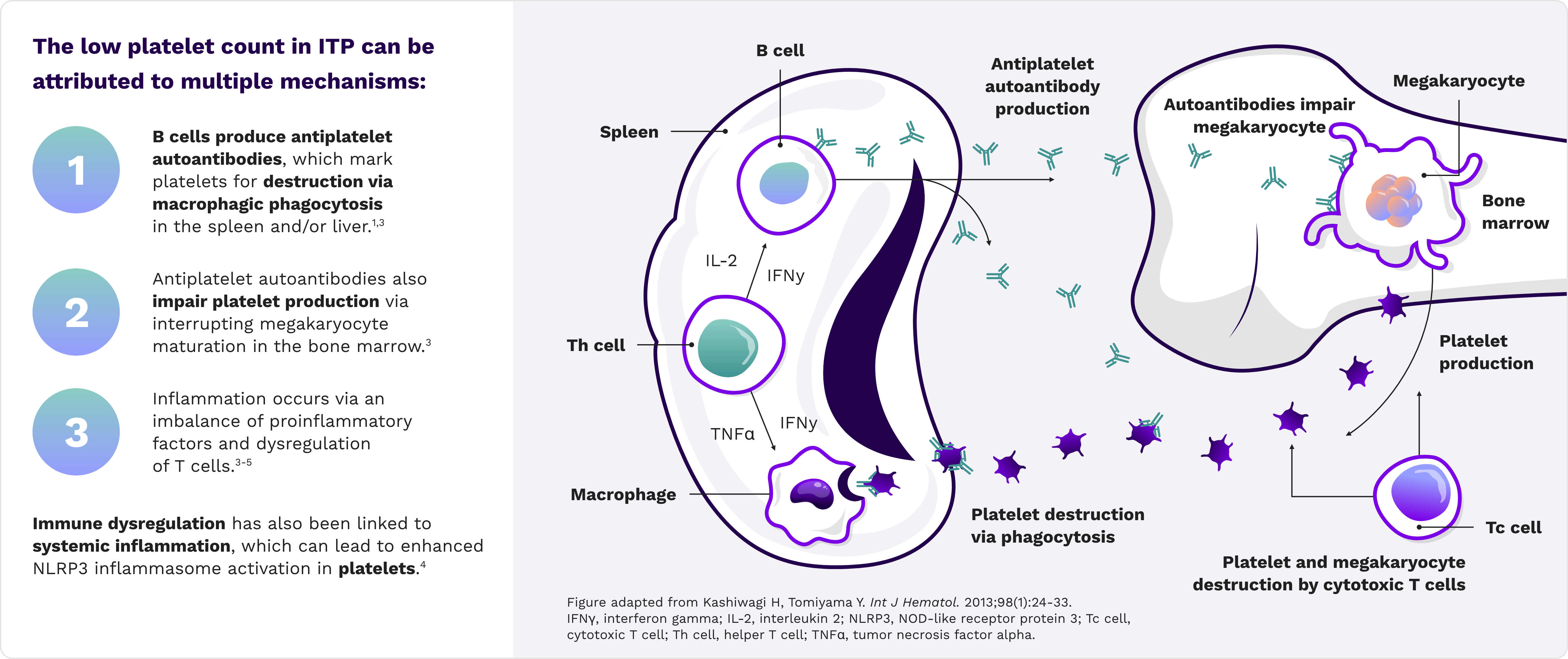
ITP is a disease of generalized immune dysregulation1,2
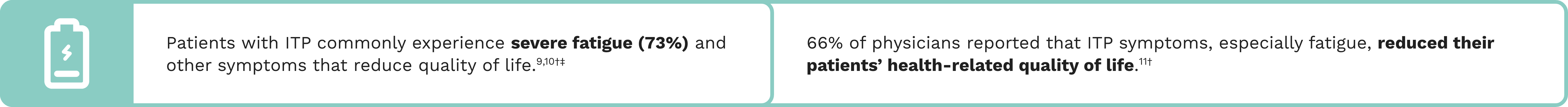
ITP causes bleeding and significantly impacts quality of life
![]()
Bleeding occurs in ~60% of patients; severe bleeding occurs in ~7% of patients6,7*
In patients aged >60 years, intracerebral
hemorrhage is the most common ITP-related cause of death, with a 50% to 80% mortality rate8
*As seen in a cross-sectional study of 302 French patients enrolled in clinical registries.
†Results from the international online ITP World Impact Survey (I-WISh), a cross-sectional survey of patients with ITP and treating hematologists or hemato-oncologists from 13 countries (Canada, China, Colombia, Egypt, France, Germany, India, Italy, Japan, Spain, Turkey, United Kingdom, and United States), completed by 1,507 patients and 472 physicians between December 2017 and August 2018.
‡Results from a study of 69 patients with ITP with a nadir platelet count of <30,000/μL.
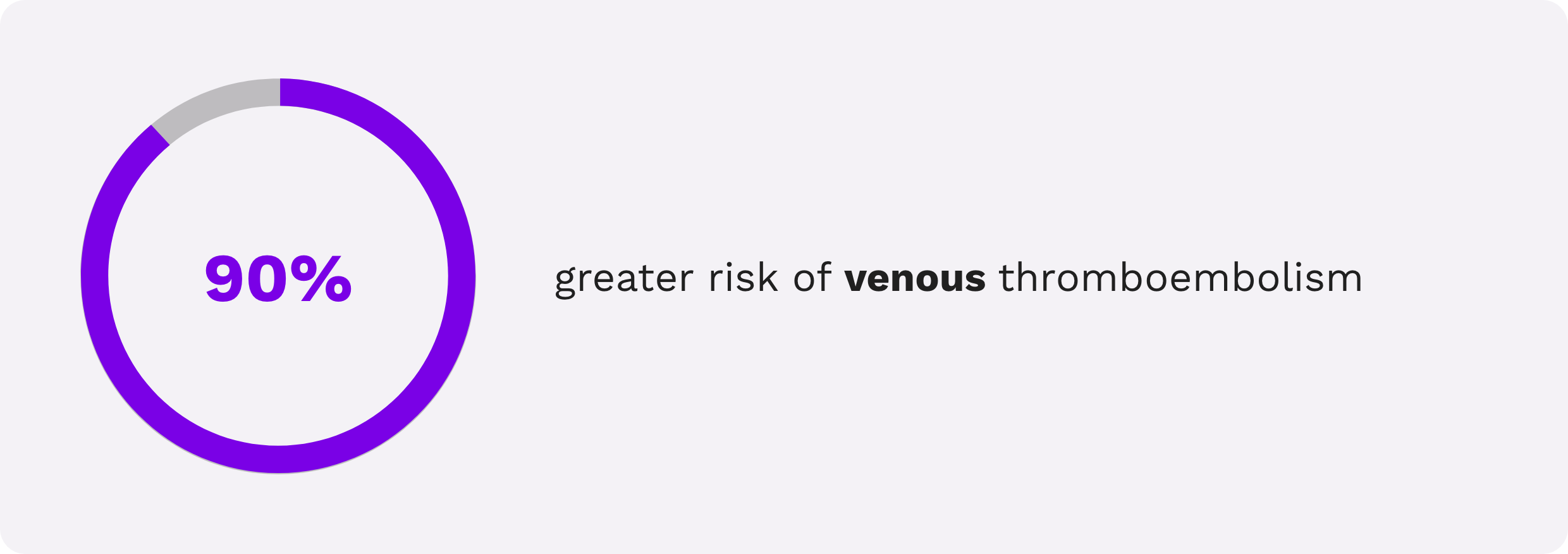
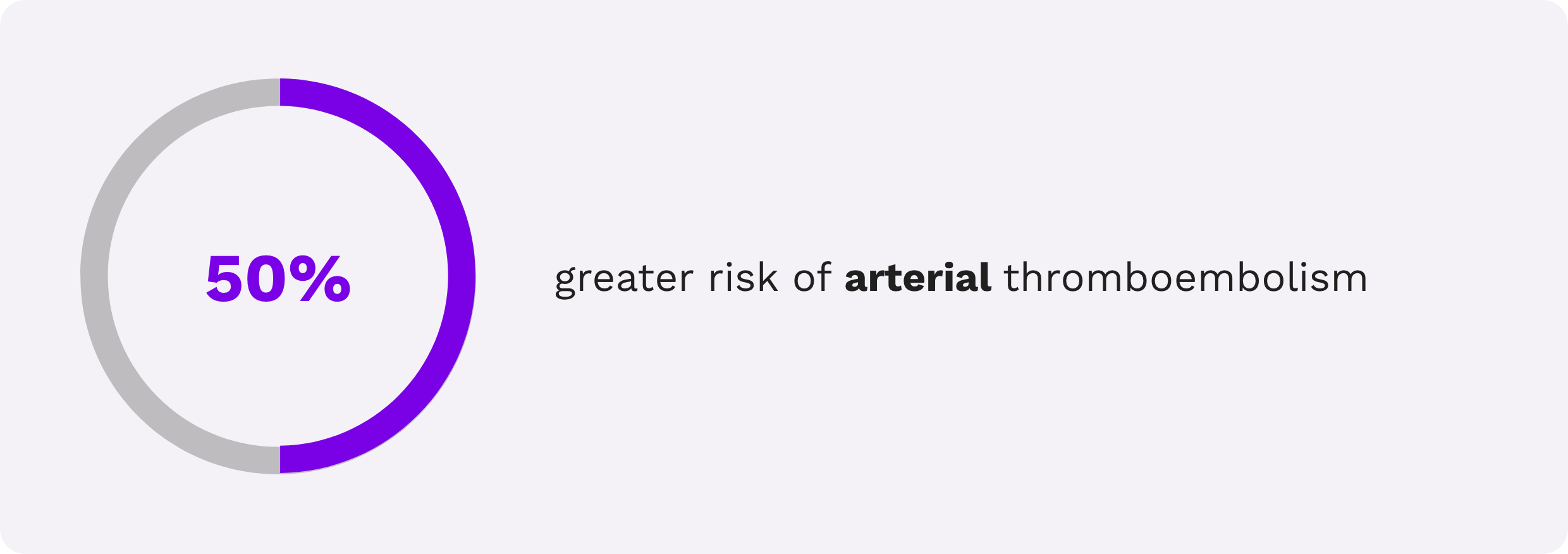
Patients with ITP have an increased risk of thrombosis12,13
Several large-scale population-based studies have shown that patients with ITP have an increased risk of arterial and venous thrombosis compared with the general population.12,13
In a meta-analysis of 5 population-based observational studies from Denmark, the United Kingdom, the United States, and Sweden, compared with the general population, patients with ITP (N=10,376) had13:
Study limitations: Relative risk was used as the primary measure of effect rather than rate difference. ITP was defined differently across studies with no distinction between newly diagnosed, persistent, or chronic ITP. Thrombotic events were defined differently and had different exclusion criteria across studies. There was no stratification by splenectomy status. Patients with ITP included in the observational studies were likely to have less severe disease than those in experimental clinical trials.
ITP is confirmed by diagnosis of exclusion14
ITP SYMPTOMS AND SYMPTOM SEVERITY VARY FROM PATIENT TO PATIENT
| PLATELET COUNT | Clinical overview1,15-17 |
|---|---|
| 150–450 × 10⁹/L | Normal platelet count in adults |
| <100 × 10⁹/L | Platelet count for patients with ITP |
| <20 × 10⁹/L | Platelet count when ITP is often diagnosed |
| <10 × 10⁹/L | Risk of severe bleeding, including intracranial and other internal bleeding |
ITP has 3 distinct disease phases after diagnosis14
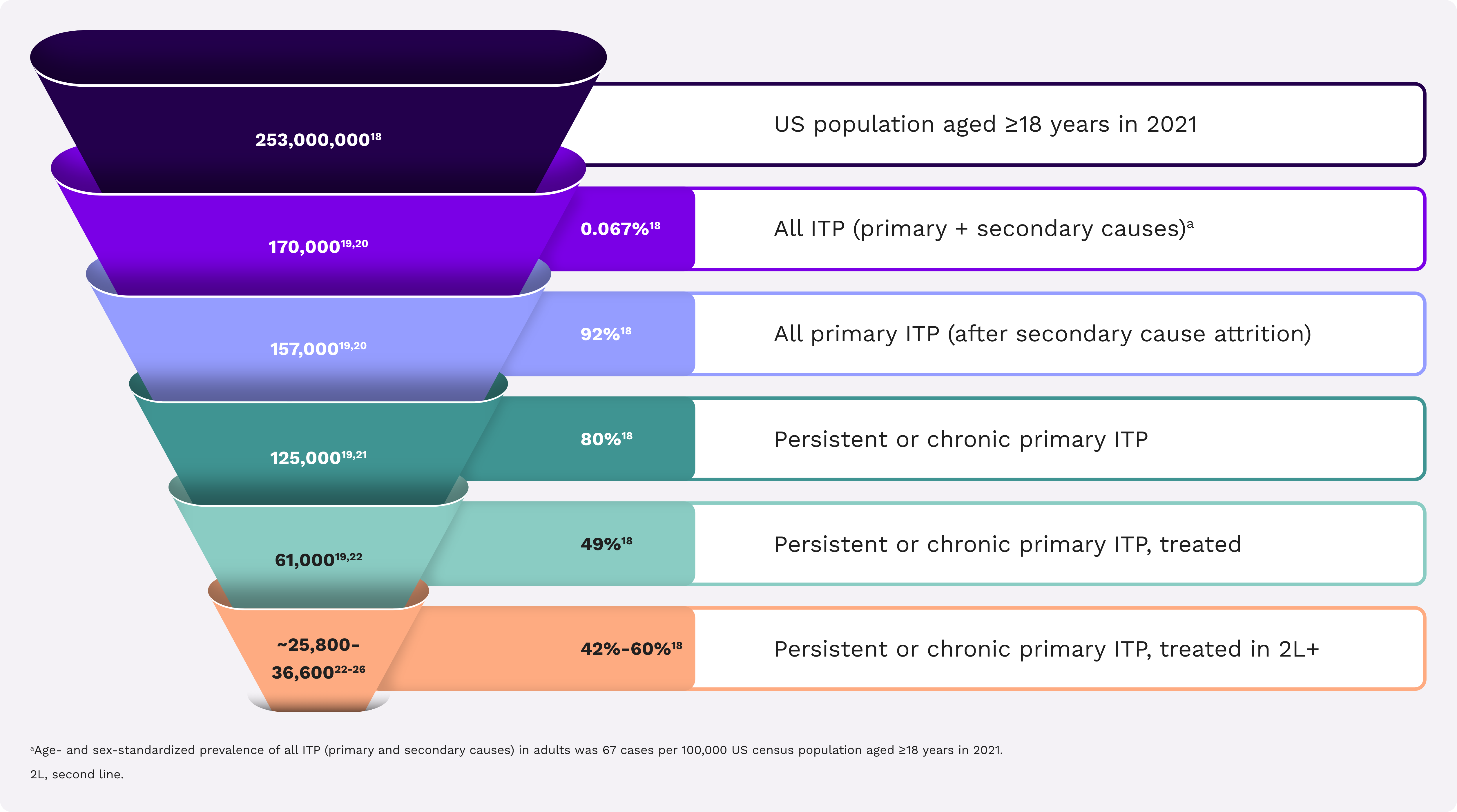
ITP is a rare disease in the United States18-26
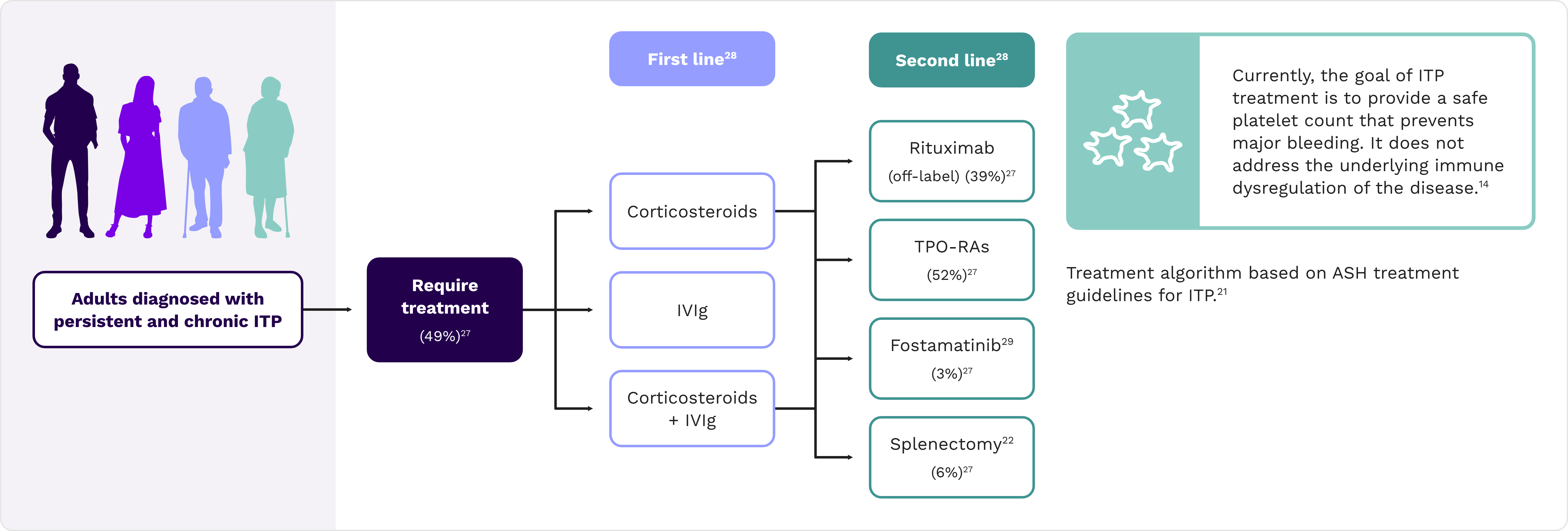
Half of patients with persistent or chronic ITP require treatment
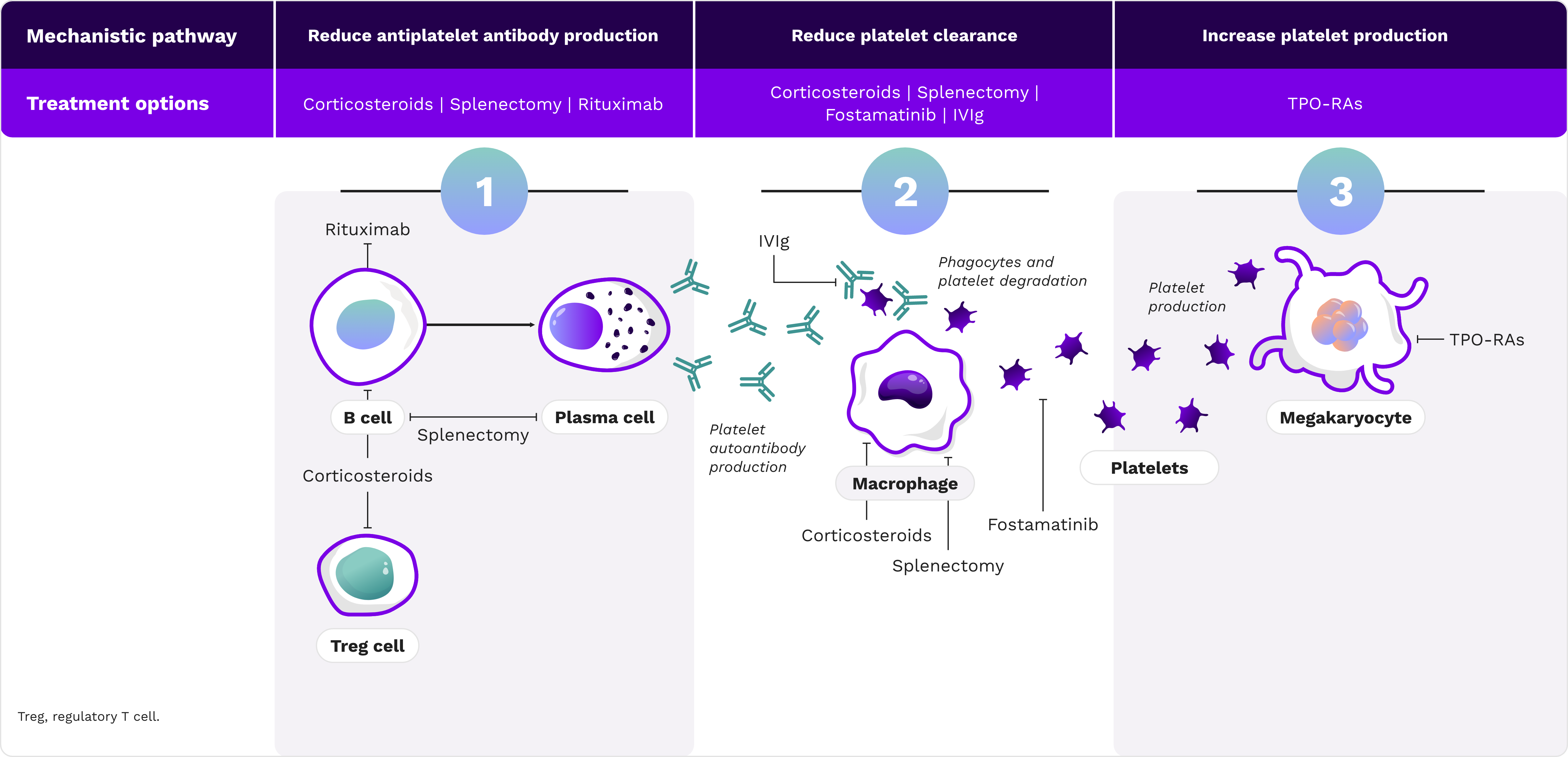
The heterogeneous nature of ITP creates the need for multiple treatment options.
ASH, American Society of Hematology; IVIg, intravenous immunoglobulin; TPO-RA, thrombopoietin receptor agonist.
ITP-related hospitalizations are typically long and costly30*
As the US population continues to age, ITP-related hospitalizations could further increase.
Over a 7-year period, there were an estimated 296,870 ITP-related hospitalizations
Causes for ITP-related hospitalization included coagulation disorder, splenectomy,† septicemia, gastrointestinal hemorrhage, intracranial hemorrhage, and epistaxis
Each ITP-related hospital stay was an average of 6 days, which was 28% longer than the average length of all other hospital stays in the United States

The average cost of an ITP-related hospitalization was $22,428,‡ which was 48% higher than the average cost of all other hospital stays in the United States
Total ITP-related hospitalization cost over the 7-year period was $6.7 billion, or approximately $960 million annually†
*A retrospective analysis of US hospital data from 2006 to 2012 examining the length of stay, hospitalization cost, and risk of in-hospital mortality among US adult patients with ITP.
†In this study splenectomy was used as a treatment option for ITP.
‡Converted to 2024 US dollars.
Currently available treatments do not provide comprehensive disease control31
Exclusive, near-term pipeline information for payers only
Designed specifically to support your early formulary decisions

Unlock access to our featured pipeline product investigating ITP*
*This content is exclusive to population-based decision makers. If your email is auto-verified, you will be granted immediate access. If you are not auto-verified, registration is required.
References: 1. Cooper N, Ghanima W. Immune thrombocytopenia. N Engl J Med. 2019;381(10):945-955. doi:10.1056/NEJMcp1810479 2. Machlus KR, Italiano JE Jr. The incredible journey: from megakaryocyte development to platelet formation. J Cell Biol. 2013;201(6):785-796. doi:10.1083/jcb.201304054 3. Kashiwagi H, Tomiyama Y. Pathophysiology and management of primary immune thrombocytopenia. Int J Hematol. 2013;98(1):24-33. doi:10.1007/s12185-013-1370-4 4. Wang M, Chen Z, Wong M, et al. Are the correct outcomes being measured in studies of oral anticoagulants? A systematic survey. Thromb Res. 2021;201:30-49. doi:10.1016/j.thromres.2021.02.016 5. Nelson VS, Jolink ATC, Amini SN, et al. Platelets in ITP: victims in charge of their own fate? Cells. 2021;10(11):3235. doi:10.3390/cells10113235 6. Piel-Julian ML, Mahévas M, Germain J, et al. Risk factors for bleeding, including platelet count threshold, in newly diagnosed immune thrombocytopenia adults. J Thromb Haemost. 2018;16(9):1830-1842. doi:10.1111/jth.14227 7. Audia S, Bonnotte B. Emerging therapies in immune thrombocytopenia. J Clin Med. 2021;10(5):1004. doi:10.3390/jcm10051004 8. Al-Samkari H, Kuter DJ. Immune thrombocytopenia in adults: modern approaches to diagnosis and treatment. Semin Thromb Hemost. 2020;46(3):275-288. doi:10.1055/s-0039-1700512 9. Cooper N, Kruse A, Kruse C, et al. Immune thrombocytopenia (ITP) World Impact Survey (iWISh): patient and physician perceptions of diagnosis, signs and symptoms, and treatment. Am J Hematol. 2021;96(2):188-198. doi:10.1002/ajh.26045 10. Vladescu C, Hart ACJ, Paul D, et al. Cognitive impairment in patients with immune thrombocytopenia. Blood. 2022;140(suppl 1):5553-5554. doi:10.1182/blood-2022-166412 11. Cooper N, Kruse A, Kruse C, et al. Immune thrombocytopenia (ITP) World Impact Survey (I-WISh): impact of ITP on health-related quality of life. Am J Hematol. 2021;96(2):199-207. doi:10.1002/ajh.26036 12. Swan D, Newland A, Rodeghiero F, Thachil J. Thrombosis in immune thrombocytopenia – current status and future perspectives. Br J Haematol. 2021;194(5):822-834. doi:10.1111/bjh.17390 13. Langeberg WJ, Schoonen WM, Eisen M, Gamelin L, Stryker S. Thromboembolism in patients with immune thrombocytopenia (ITP): a meta-analysis of observational studies. Int J Hematol. 2016;103(6):655-664. doi:10.1007/s12185-016-1974-6 14. Rodeghiero F, Stasi R, Gernsheimer T, et al. Standardization of terminology, definitions and outcome criteria in immune thrombocytopenic purpura of adults and children: report from an international working group. Blood. 2009;113(11):2386-2393. doi:10.1182/blood-2008-07-162503 15. Zufferey A, Kapur R, Semple JW. Pathogenesis and therapeutic mechanisms in immune thrombocytopenia (ITP). J Clin Med. 2017;6(2):16. doi:10.3390/jcm6020016 16. Vrbensky JR, Moore JE, Arnold DM, Smith JW, Kelton JG, Nazy I. The sensitivity and specificity of platelet autoantibody testing in immune thrombocytopenia: a systematic review and meta-analysis of a diagnostic test. J Thromb Haemost. 2019;17(5):787-794. doi:10.1111/jth.14419 17. Schoonen WM, Kucera G, Coalson J, et al. Epidemiology of immune thrombocytopenic purpura in the General Practice Research Database. Br J Haematol. 2009;145(2):235-244. doi:10.1111/j.1365-2141.2009.07615.x 18. Age and sex composition in the United States: 2021. United States Census Bureau. Accessed June 12, 2025. https://www.census.gov/data/tables/2021/demo/age-and-sex/2021-age-sex-composition.html 19. Data on file. Optum database, 2023 analysis of 2021 population. Sanofi. 20. Doobaree IU, Conway K, Miah H, et al. Incidence of adult primary immune thrombocytopenia in England—an update. Eur J Haematol. 2022;109(3):238-249. doi:10.1111/ejh.13803 21. Neunert C, Terrell DR, Arnold DM, et al. American Society of Hematology 2019 guidelines for immune thrombocytopenia. Blood Adv. 2019;3(23):3829-3866. doi:10.1182/bloodadvances.2019000966 22. Provan D, Arnold DM, Bussel JB, et al. Updated international consensus report on the investigation and management of primary immune thrombocytopenia. Blood Adv. 2019;3(22):3780-3817. doi:10.1182/bloodadvances.2019000812 23. González-López TJ, Schifferli A. Early immunomodulation in immune thrombocytopenia—a report of the ICIS meeting in Lenzerheide, Switzerland 2022. Br J Haematol. 2023;203(1):101-111. doi:10.1111/bjh.19082 24. Witkowski M, Witkowska M, Robak T. Autoimmune thrombocytopenia: current treatment options in adults with a focus on novel drugs. Eur J Haematol. 2019;103(6):531-541. doi:10.1111/ejh.13319 25. Wei Y, Ji XB, Wang YW, et al. High-dose dexamethasone vs prednisone for treatment of adult immune thrombocytopenia: a prospective multicenter randomized trial. Blood. 2016;127(3):296-302, 370. doi:10.1182/blood-2015-07-659656 26. Data on file. ITP – rilzabrutinib demand assessment, US 2023. Sanofi. 27. Data on file. Sanofi. 28. Provan D, Stasi R, Newland AC, et al. International consensus report on the investigation and management of primary immune thrombocytopenia. Blood. 2010;115(2):168-186. doi:10.1182/blood-2009-06-225565 29. Bussel J, Arnold DM, Grossbard E, et al. Fostamatinib for the treatment of adult persistent and chronic immune thrombocytopenia: results of two phase 3, randomized, placebo-controlled trials. Am J Hematol. 2018;93(7):921-930. doi:10.1002/ajh.25125 30. An R, Wang PP. Length of stay, hospitalization cost, and in-hospital mortality in US adult inpatients with immune thrombocytopenic purpura, 2006-2012. Vasc Health Risk Manag. 2017;13:15-21. doi:10.2147/VHRM.S123631 31. Singh A, Uzun G, Bakchoul T. Primary immune thrombocytopenia: novel insights into pathophysiology and disease management. J Clin Med. 2021;10(4):789. doi:10.3390/jcm10040789
This site is intended for US payers only.
© 2025 Sanofi. All rights reserved.